One in six bacterial infections worldwide in 2023 no longer respond to common antibiotic treatments, according to a new World Health Organization (WHO) report released today.
Between 2018 and 2023, antibiotic resistance increased in more than 40% of the pathogen–antibiotic combinations tracked by WHO, with annual growth rates ranging from 5% to 15%. Data collected through the Global Antimicrobial Resistance and Use Surveillance System (GLASS) from over 100 countries show that rising resistance to essential antibiotics poses an escalating threat to global health.
The Global Antibiotic Resistance Surveillance Report 2025 presents, for the first time, global estimates of resistance prevalence across 22 antibiotics used to treat urinary, gastrointestinal, bloodstream, and sexually transmitted infections, including gonorrhoea.
Eight major bacterial pathogens were analyzed in the report: Acinetobacter spp., Escherichia coli, Klebsiella pneumoniae, Neisseria gonorrhoeae, non-typhoidal Salmonella spp., Shigella spp., Staphylococcus aureus, and Streptococcus pneumoniae—each associated with one or more serious infections.
Regional differences in antibiotic resistance
WHO estimates indicate that resistance is highest in the South-East Asian and Eastern Mediterranean regions, where one in three infections are antibiotic-resistant. In the African Region, one in five infections show resistance. Resistance levels are particularly severe in areas with weak health systems and limited diagnostic or treatment capacity.
“Antimicrobial resistance is outpacing advances in modern medicine, threatening the health of families worldwide,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “We must use antibiotics responsibly and ensure equitable access to effective medicines, diagnostics, and vaccines. Strengthening prevention, diagnosis, and treatment systems, and developing next-generation antibiotics and rapid tests, are crucial to our shared future.”
Gram-negative bacteria driving the crisis
The report highlights Gram-negative bacterial pathogens as the most pressing threat. Drug-resistant E. coli and K. pneumoniae—common causes of bloodstream infections—are leading contributors to severe illness, sepsis, and death.
Globally, more than 40% of E. coli and 55% of K. pneumoniae strains are resistant to third-generation cephalosporins, the first-line treatment for these infections. In the African Region, resistance exceeds 70%.
Other essential antibiotics, including carbapenems and fluoroquinolones, are also losing effectiveness against E. coli, K. pneumoniae, Salmonella, and Acinetobacter. Carbapenem resistance, once rare, is now increasing, forcing reliance on costly last-resort drugs that remain scarce in low- and middle-income countries.
Progress in surveillance, but gaps remain
Global participation in WHO’s GLASS program has grown from 25 countries in 2016 to 104 in 2023. Yet, nearly half of all countries did not submit data in 2023, and many still lack the capacity to generate reliable information.
The report underscores that countries most affected by antimicrobial resistance are often the least equipped to monitor or respond. The 2024 UN Political Declaration on AMR calls for stronger health systems and a “One Health” approach—integrating human, animal, and environmental health efforts to curb resistance.
WHO urges all countries to submit high-quality AMR and antibiotic use data to GLASS by 2030, emphasizing the need for stronger surveillance networks, improved laboratory systems, and evidence-based treatment guidelines aligned with local resistance patterns.
The report is accompanied by expanded digital content on WHO’s GLASS dashboard, which features global and regional summaries, country-specific profiles, and detailed data on antimicrobial resistance and usage trends.
UNICEF Condemns Killing of 17 Children in RSF Attack on Displacement Centre in North Darfur
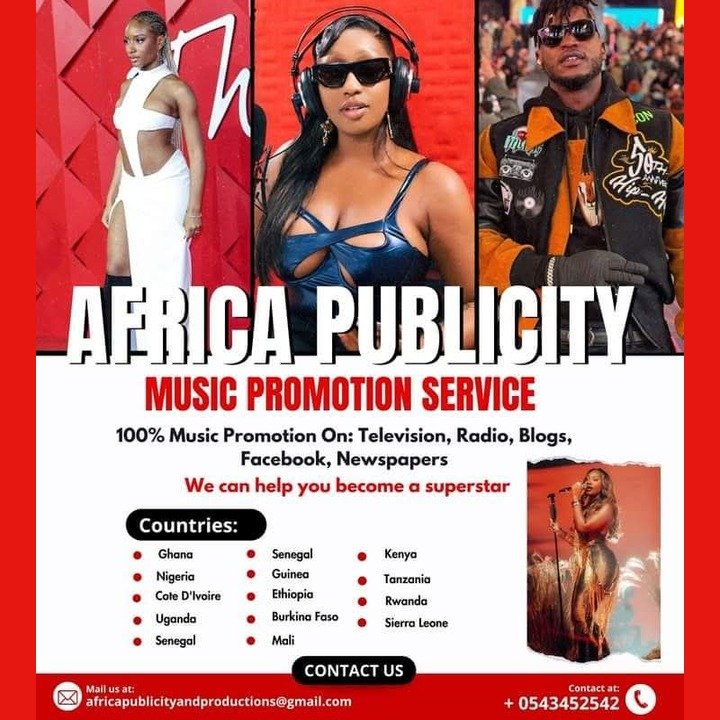
Source:Africa Publicity